Breast augmentation or breast reconstruction with breast implants carries associated risks and complications, which should be carefully considered. Breast implant illness (BII) is the term used to describe a wide range of symptoms that have been reported by patients, after receiving breast implants. Over the past two decades, multiple studies have been conducted to investigate if there is a relationship between breast implants and a wide range of symptoms including cancer, connective tissue disease, rheumatology symptoms, autoimmune diseases, fatigue, neurological disorders, difficulty conceiving, and mental health disorders.
The History of Breast Implants and Breast Implant Illness
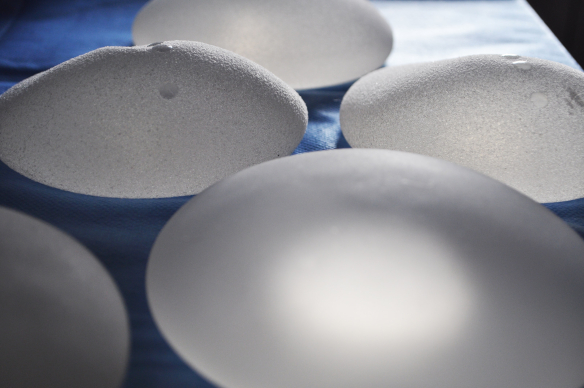
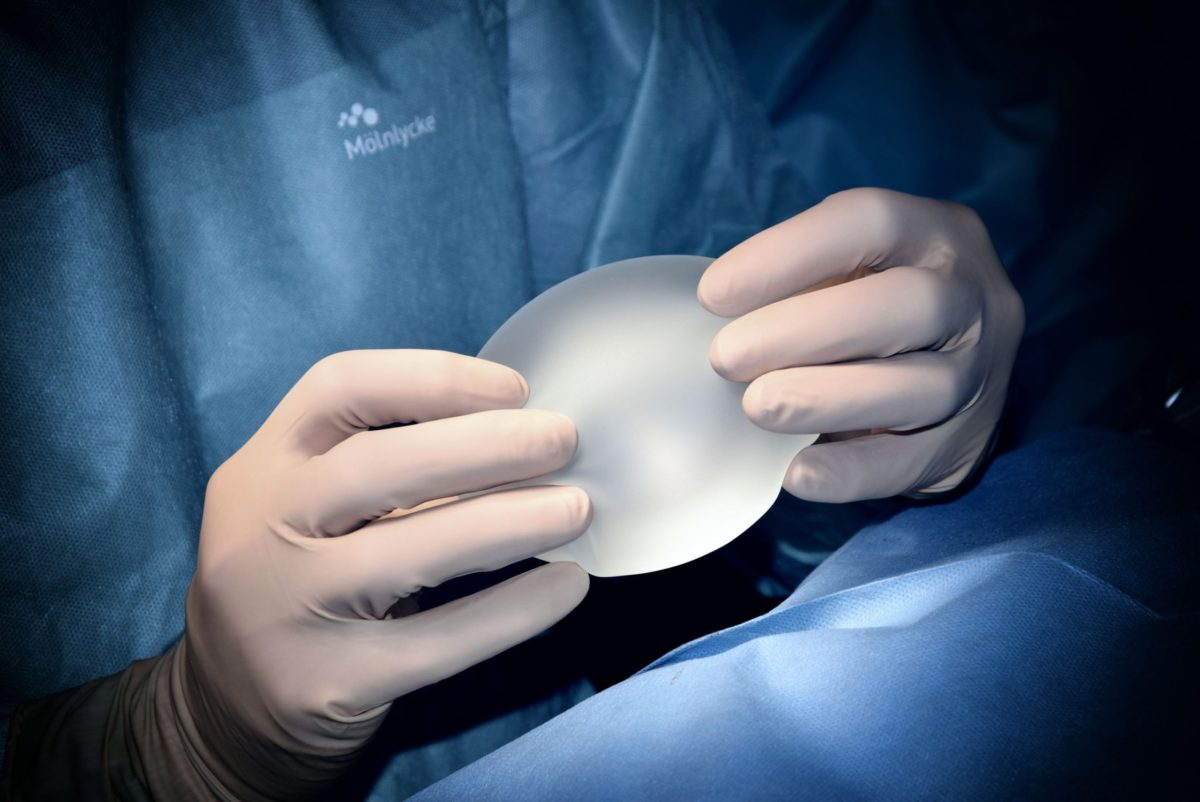
The first breast implants were invented by the surgeons, Thomas Cronin and Frank Gerow, in 1962. The first breast implants had a silicone shell and were filled with medical-grade silicone gel and manufactured by Dow Corning. The silicone gel was liquid in nature and could leak if the breast implants ruptured and may also have leaked even on intact and undamaged breast implants, through the actual breast implant shell, which was thinner than today’s breast implants. Breast augmentation with the new silicone breast implants was extremely popular and when various complications were reported, a number that could be directly associated with silicone leaking, such as granulomas, infections, and capsular contraction, which could be painful and make women with breast implants feel unwell. The result was hundreds of lawsuits brought against Dow Corning and the FDA restricting the use of silicone in April 1992. This restriction did not, as many people thought, totally ban the use of silicone-filled implants in the U.S.A; the FDA restriction did not apply to reconstructive procedures or women who requested silicone-filled, breast implants for secondary breast augmentation procedures.
The FDA restrictions in the USA were not followed by many other countries including the UK, where the MHRA did not find any concern over the safety of silicone-filled breast implants and women continued to receive silicone-filled breast implants, for initial breast augmentation procedures. In the USA, saline-filled, breast implants replaced silicone-filled breast implants, although even silicone breast implants were manufactured with a silicone outer shell. Numerous studies were conducted and continued to show that there was no direct link that could be established between silicone-filled breast implants and the symptoms women with breast implants were reporting. Based on the epidemiological data in 2006 the FDA lifted the restrictions. Silicone-filled breast implants from this point could be used for primary, breast augmentation procedures. Women around the world continued to report symptoms of BII and the research continued to evaluate the safety of both, silicone-filled and saline-filled breast implants.
Silicone-filled breast implants were requested significantly more than saline breast implants in the UK and data continued to show that there was no greater occurrence of symptoms, referred to as BII, reported by women with breast implants. In the UK substances for breast implants also included Trilucent soya ‘gel’, and Hydrogel. However, they were both withdrawn from use and also recalled in the UK following high levels of complications, including bleeding/leakage of the soya through the breast implant shell and a lack of data from biological safety assessments. In the UK and the USA, the only two fillings now used for breast implants are silicone and saline. However, both saline and silicone-filled breast implants, have a silicone shell. Silicone breast implants continue to be the most popular choice in both the UK and the USA.
Women continue to report symptoms of BII. There are also many women, who say, after their breast implants were removed, the symptoms of BII, either reduced or stopped completely. Consequently, the media have used these women to sell stories with dramatic headings like the article on the BBC website ‘My breast implants made me feel like I was dying’ by Anna Hodges, Newsbeat BBC and ‘Mother-of-three, 45, who wanted breast implants to perk up her ‘pitiful’ boobs reveals they made her so ill she thought she was DYING’ by Claire Toureille, Mail Online. What the media didn’t say is that the data showed the same level of BII symptoms in women without breast implants. BII is NOT recognised by the World Health Organisation.
Reports and Research into Breast Implant Illness (BII)
A 440-page report of a study on breast implants by the Institute of Medicine (IOM) into the safety of silicone-filled breast implants systematically reviewed various research and studies. The aim was to objectively assess all of the evidence of breast implants causing illness to women, their unborn babies, and if there was an increase of silicone in breastmilk.
The report found that in women with both silicone-filled and saline-filled breast implants there was:
No elevated risk of connective tissue disease or rheumatic conditions
No increased incidence of neurological diseases
No evidence of higher silicone levels in breast milk, than in women without breast implants
No evidence that women with breast implants report higher levels of birth defects
No significant evidence that radiation therapy is less effective in women with breast implants
BII and the Poly Implant Prothese (P.I.P) breast implants fraud
In March 2010, P.I.P breast implants, made in France, were withdrawn after it was revealed they had been filled with industrial-grade, silicone instead of medical-grade silicone. This was not an issue about the safety of medical-grade, silicone-filled, breast implants; however, it is a concern that any manufactures of breast implants would commit fraud and that breast implants were given an EU certification for years when they had not been made to the EU standards.
If you have P.IP breast implants that have not ruptured you should have regular mammograms if you do not have them removed. If you do want your P.I.P breast implants removed then you should contact the surgeon who did your breast surgery. Below are the companies that have agreed to offer removal and replacement of P.I.P breast implants for no charge:
Make Yourself Amazing/MYA Cosmetic Surgery
In the Uk, you may also be able to have P.IP implants removed by the NHS. The NHS may not provide replacement breast implants unless you had breast reconstruction surgery with breast implants.
However, the NHS may provide removal and replacement of P.I.P breast implants, if your breast surgery was done initially by the NHS. You may also be eligible to claim compensation if your P.I.P breast implants rupture and you have health problems that could be related
Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)
In July 2019 Allergan withdraw from the worldwide market all textured breast implants due to a link to Breast implant-associated anaplastic large cell lymphoma – BIA-ALCL is a rare type of T-cell lymphoma (cancer of the immune system). This was the first time a definitive link had been made between cancer and breast implants that is recognised by the World Health Organisation. If you do not know the manufacturer of your breast implants, or if they have a textured shell contact your plastic surgeon who should be able to provide this information. If you can not reach your plastic surgeon then you should monitor for symptoms of BIA-ALCL.
Symptoms of BIA-ALCL
The main symptoms of BIA-ALCL include:
Swelling of breasts
Hardening of breasts
Pain in breasts or close to breasts such as underarms
Feeling of heat in your breasts
Redness or rash around breasts or nearby
Change in shape
Lumps in breast or armpit
Fatigue
Sudden unexplained weight loss
Even if you do not have any symptoms of BIA-ALCL you can request a physical examination with your plastic surgeon which should be free of charge. If your plastic surgeon is concerned they may then request an ultrasound or an MRI. When fluid or a mass is detected your plastic surgeon should then perform a needle biopsy to take some of the fluid to test for CD30 immune staining (CD30IHC). When CD30IHC is found this is a diagnosis of BIA-ALCL, however, this test does not always detect CD30IHC, which means it is possible to have BIA-ALCL without knowing if there are no symptoms. When symptoms are apparent even if CD30IHC is not found, you may want to consider removing and replacing your breast implants (especially if they have a textured shell).
If you do have breast implants with a textured shell, regardless of whether they are filled with saline or silicone you may be able to file a lawsuit. For more information please look at this blog post.
My Opinion
I think it is unlikely there are links between almost all symptoms of BII and breast implants. Additionally, I have always questioned the FDA’s restriction of the use of silicone-filled breast implants. It seems incomprehensible that the FDA allowed silicone-filled breast implants to be used for secondary breast augmentation or reconstructive procedures if they were considered not safe? There have been isolated studies that show a connection between BII and breast implants, yet they certainly don’t demonstrate a definite link between BII and breast implants. It is likely as with all medicine and medical products, that a small percentage of patients may experience symptoms of BII and benefit from having breast implants removed.
Annabelle Baugh | Founder