Safety and Health Related Issues
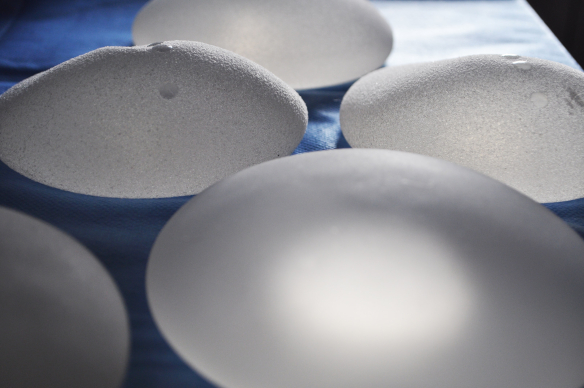
Breast implant safety has been a source of contention for many years. Women began to report a wide range of health complications within months of silicone filled breast implants becoming widely accessible.
Following a number of successful lawsuits, the Food and Drug Administration US (FDA) restricted the use of silicone filled breast implants in the United States in April 1992. It’s critical to note that the FDA never prohibited the use of silicone filled breast implants, only limiting usage to secondary breast augmentation or reconstructive purposes.
In Europe and many other countries the use of silicone filled breast implants has never been limited. In countries that permitted unrestricted use of silicone filled breast implants, they were generally considered superior to saline filled implants.
Breast Implant Illness (BII)
Breast implant illness (BII) is not one condition but a wide range of systemic symptoms. In 2006 following extensive research which could not prove a definitive link between silicone filled breast implants and reported health issues, the FDA lifted all restrictions on the use of silicone filled breast implants.
In addition to researching silicone filled breast implants, numerous studies have assessed if there are any links between health issues reported by women after having saline filled breast implants. As with silicone filled breast implants no definitive links have been found between silicone filled breast implants and reported health issues.
The US Food and Drug Administration (FDA) and the UK Medicines and Healthcare products Regulatory Agency (MHRA) have also put information about BII on their respective websites.
Additional types of implants licensed for use in the UK and Europe, which were withdrawn are trilucent soya implants and hydrogel implants and Poly Implant Prothese (PIP) implants, due to concerns about their long term safety.
Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)
In July 2019 breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) resulted in the worldwide withdrawal of BIOCELL textured, Allergan breast implants. BIA-ALCL is cancer of the lymphatic system, caused by a rare type of T-cell lymphoma and it can develop with both silicone or saline filled textured breast implants.
The rate of BIA-ALCL is estimated to be less than 0.1% according to the most recent research published by the Scientific Committee on Health, Environmental and Emerging Risks (SCHEER) which found the estimated lifetime incidence ranges from from 1.65 to 35 instances per 100,000 people who have received breast implants.
According to new data published in a paper in October of 2021, 28 occurrences of BIA-ALCL are linked to smooth breast implants. Out of them, only one instance had a history of using only implants with smooth shells. All of the remaining occurrences involved patients who either had prior exposure to textured breast implants or had no recorded history. Tissue expander devices and BIA-ALCL have not yet been linked in any known occurrences.
BIA-ALCL can occur years after successful breast augmentation, even if you did not have any complications following your breast augmentation procedure. The FDA AND MHRA are not recommending removing or replacing textured or polyurethane-coated implants and currently advise to be aware of symptoms of BIA-ALCL including:
- Swelling
- Pain
- Lumps
- Skin changes
- Changes in breast shape
If you have any symptoms or concerns speak with your plastic surgeon or another medical professional immediately. According to research published in a medical journal, The Breast, in December 2022, clinical guidelines for diagnosis and treatment of BIA-ALCL are as follows
- When any symptoms are present an ultrasound-guided fine-needle aspiration of the fluid in the capsule surrounding the implant should be performed. This should then be sent for pathology tests.
- Treatment for BIA-ALCL is en bloc capsulectomy with implant removal.
- In patients with stage two, three or four BIA-ALCL that extends beyond the capsule and has lymph node involvement, full excision of the tumor mass and lymphadenectomy is the recommended surgical strategy. This should be followed by chemotherapy and immunotherapy.
- Autologous tissue reconstruction, either immediate or delayed, should be chosen over breast implants for patients diagnosed with BIA-ALCL
Breast Implants and Cancer
On September 8, 2022, the US Food and Drug Administration (FDA) issued a safety communication on reports of squamous cell carcinoma (SCC) and other lymphomas present in the scar tissue capsule that surrounds breast implants. These lymphomas are distinct from BIA-ALCL. Even though the tumors seem to be extremely rare, they have been linked to textured and smooth implant shells.
The FDA received 24 medical device reports (MDRs) involving SCC with breast implants as of January 15, 2023, according to the most recent FDA update on March 8th, 2023. This update additionally provided new advice for healthcare professionals in relation to implants and the management of SCC or lymphomas found in the capsule.
The advice is as follows:
- When speaking with individuals who have or are thinking about getting breast implants, be sure to mention SCC and different lymphomas in the capsule surrounding the implant.
- Create an individualized treatment plan in collaboration with a multidisciplinary team of specialists, including surgical oncology, plastic surgery, breast surgery, radiology, oncology, and pathology, for patients who have been diagnosed with SCC or different lymphomas in the capsule surrounding the breast implant.
- Inform the FDA of any instances of SCC, lymphomas, or any other malignancies found in capsules surrounding breast implants.
Poly Implant Prothese (PIP) Breast Implants Safety Information
Following the withdrawal of PIP implants and prior to a more extensive testing programme that the French Regulatory Authority (AFSSAPS) had planned, the MHRA ordered a limited number of tests in July 2010. When selecting the tests, the MHRA sought the opinions of toxicology experts. The Ames test, which detects the presence of impurities in the gel filler material that provide a high risk of genotoxicity, and analytical chemistry were used to investigate known chemical classes of impurities in the silicone gel in PIP implants.
The evidence from the commissioned investigations into the safety of PIP implants, in the opinion of an independent expert hired by the MHRA, showed that PIP silicone compounds were not carcinogenic and were not mutagenic (did not cause DNA mutations that may lead to the development of certain conditions.)
However, the investigations discovered that PIP implants are:
- Two to six times more likely than other kinds of silicone implants to rupture or bleed silicone gel after five years.
- Implant gel bleeding or ruptures in certain patients has been linked to an inflammatory reaction, either locally or in surrounding lymph nodes.
- Breast cancer or breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) have not been linked to PIP implant rupture or local inflammation.
These conclusions were subsequently confirmed in a report published June 2011 that analyzed the outcomes of the more extensive investigations carried out by the AFSSAPS (French Health Products Safety Agency) which became the ANSM (National Agency for the Safety of Drugs and Health Products) in December 2011
This has been further backed by the Safety of Poly Implant Prothèse (PIP) Silicone Breast Implants (2013 update) from the Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR). The SCENIHR stated that removal is recommended in cases of implant rupture; however, no credible medical, toxicological, or other data exist that would support routine removal of intact PIP implants.
Breast Implants and Breast Cancer
Concern about a link between breast implants, especially silicone filled implants and breast cancer has been extensively researched. According to numerous epidemiological studies there is not a higher risk of developing breast cancer associated with silicone breast implants.
Interestingly one clinical study, published in the Plastic and Reconstructive Surgery Journal in August 2021, has indicated ‘women with breast implants have heightened antibody responses to the specific breast cancer antigens mammaglobin-A and mucin-1’. This suggests that breast implants may actually help to protect women from breast cancer.
Sources
Clinical recommendations for diagnosis and treatment according to current updated knowledge on BIA-ALCL – The Breast medical journal (published December 2022)
Summary report on tests performed on extracts of silicone gel filler material from PIP silicone breast implants – MHRA (published July 2010).
Safety of Poly Implant Prothèse (PIP) Silicone Breast Implants (2013 update) – SCENIHR (published May 2014)
Breast Implants: Reports of Squamous Cell Carcinoma and Various Lymphomas in Capsule Around Implants: FDA Safety Communication – FDA (published September 2022)
Silicone Breast Implants and Cancer – National Academies Press (US)Safety of Silicone Breast Implants (published 1999)
Can Breast Implants Induce Breast Cancer Immunosurveillance? An Analysis of Antibody Response to Breast Cancer Antigen following Implant Placement – Plastic and Reconstructive Surgery 148(2):p 287-298, August 2021. | DOI: 10.1097/PRS.0000000000008165 (published August 2021)
My Opinion
Based on the current research and data from clinical studies the symptoms of BII are not conclusive and removal of breast implants is not recommended. If you have textured or polyurethane-coated implants, removal prior to developing BIA-ALCL is a personal decision and might be worthwhile if you feel extreme anxiety about your implants. If you do experience any health issues that you believe could be due to your breast implants I would urge you to have all other underlying causes investigated.
Annabelle Baugh | Founder