Breast Augmentation Important Information
Breast augmentation is an invasive procedure that requires skill and should always be performed by a specialist plastic surgeon (in the U.K breast surgeons also perform Oncoplastic reconstructive breast augmentation procedures following mastectomy for breast cancer when breast surgery or breast reconstruction is performed by the NHS and are specialist surgeons in this type of surgery).
Eight Key Important Things to Know About Breast Augmentation
- Types of breast implants
- How to choose the best breast implants
- Incision options for breast augmentation
- Breast Implant Placement Options
- Mammograms with breast implants
- General or local anesthetic for breast augmentation
- Breast augmentation cost
- Breast augmentation risks and complications
Breast augmentation Surgical Options
- Breast augmentation with breast implants
- Breast augmentation with autologous fat transfer
- Breast augmentation using natural tissue (flap procedure)
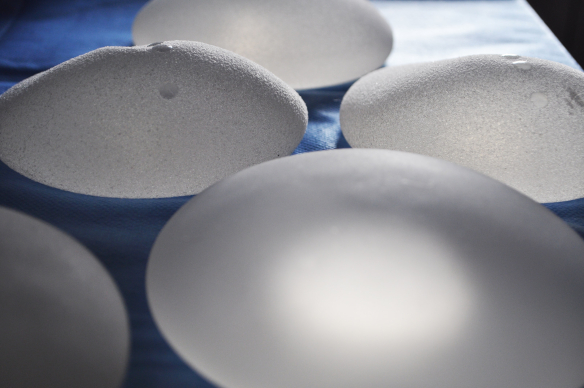
Types of Breast Implants
Silicone vs Saline Breast Implants
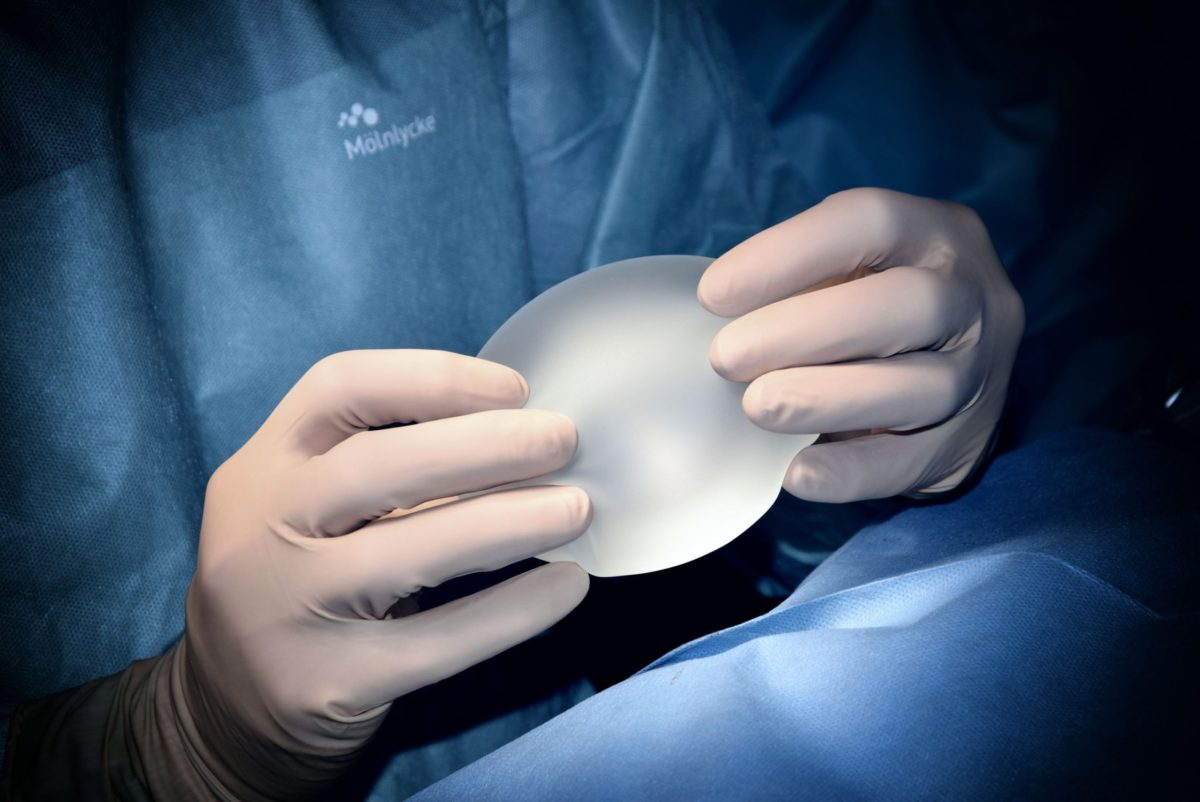
If you are considering breast augmentation with breast implants, the first decision you need to make is if you should have saline or silicone breast implants. All breast implants have an outer silicone shell and are filled with saline or silicone gel.
Saline breast implants are filled with sterile salt water and are heavier than silicone gel-filled breast implants. They are more prone to rippling and some women say they can feel the saline ‘sloshing’ inside their breast implants. Saline-filled breast implants are considered safer if they rupture, as saline is absorbed and dispelled naturally by the body.
Silicone breast implants are filled with silicone gel that comes in different consistencies and weigh less than saline-filled breast implants. The higher the consistency of the silicone gel, the firmer the breast implants feel. If silicone-filled breast implants rupture, saline can migrate into the tissues around the body.
Gummy Bear Breast Implants
The silicone gel can be thick and sticky to a more solid gel. This is referred to as the cohesivity and high cohesivity breast implants are also referred to as gummy bear breast implants. This is because the gel is similar to a jelly baby and cannot leak. Gummy bear breast implants come in both non-anatomical (round) and anatomical (teardrop). They cannot be manipulated as much as lower velocity silicone breast implants and therefore require a larger scar. Most plastic surgeons prefer to use the incision in the crease of the breast when using high cohesivity, gummy bear breast implants.
B-Lite® Breast Implants
B-Lite® Breast Implants
B-Lite® breast implants are only available in Europe and have not been given FDA approval for use in the U.S. They are available in non-anatomical (round) and anatomical (teardrop) shapes and are 30% lighter than standard silicone breast implants. They are filled with microspheres inside silicone gel and are popular for women who want to have larger breast implants and athletes or women who enjoy strenuous activities. As they are lighter it is predicted they will not sag as much as a standard silicone implant of the same size.
B-Lite® Breast Implants Video
Hydrogel breast implants
Monobloc Hydrogel breast implants are manufactured by CMC, Laboratoires Arion in France. They are currently the only biocompatible alternative to silicone-filled breast implants (excluding saline). Laboratoires Arion hydrogel breast implants have obtained the CE marking issued by the independent inspection body LNE GMED and are authorized by the AFSSAPS. They are not FDA approved and can not be used in the U.S.
Important information about Breast Implant Manufacturers.

Breast Implant Shapes
Non-anatomical ‘Round’ Breast Implants
Non- anatomical breast implants are often referred to as round breast implants and are of the same height and width. They come in various profiles and when the correctly sized breast implants are used, they can produce a natural or fake-looking breast shape, depending on the goal of the patient.
Anatomical ‘Tear Drop’ Breast Implants
Anatomical breast implants are often referred to as teardrop breast implants and have a different height to width ratio, with more volume towards the bottom of the breast implant. If you want natural looking breast implants, your plastic surgeon may recommend anatomical breast implants.
Tissue Expanders ‘Expandable’ Breast Implants’
Tissue expanders are also referred to as expandable breast implants. They were initially used for breast reconstructive surgery, following a mastectomy. Tissue expanders are gradually filled with saline, over a period of months. This allows the skin and muscles to stretch over time. There are permanent tissue expanders or temporary ones, that are normally replaced with prefilled silicone breast implants. Due to a demand for extra-large breast implants, tissue expanders are now also used for breast augmentation procedures. Another type of tissue expander has a saline lumen inside a silicone gel lumen. The silicone gel lumen helps to prevent visible rippling.
All tissue expanders or expandable breast implants have higher associated complications and infection rates. This is due to the external port, normally in the armpit that is required for adding saline. Warranties also become void when tissue expanders are overfilled.
Breast Implant Profiles
The profile of breast implants refers to the distance the breast implant projects from the chest wall.
Breast implants come in low to extra high profiles. High profile non-anatomical (round) breast implants are rounder in shape.
Breast Implant Volumes
Breast implant volume refers to the size and is measured in cubic centimeters (cc). Breast implants are available in a wide range of cc volumes up to 800cc. Saline-filled breast implants can be overfilled to greater than 800cc. Silicone-filled breast implants over 800cc need to be custom made.
Saline breast implants can be overfilled, however, this will usually void any warranty.
Breast Implant Textures
The outer shells of all breast implants are made of silicone and can be smooth or textured.
Textured shells tend to be used for anatomical breast implants, to prevent the breast implants from rotating. They have been linked to a rare type of T-cell lymphoma (cancer of the immune system). Called breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) this has been linked to saline and silicone-filled textured breast implants.
How Long do Breast Implants Last?
Breast implants now usually come with a lifetime warranty. Previously breast implants were thought to last 10 years, however, this is no longer the case with the newer generation of silicone breast implants. Saline breast implants are more likely to rupture and need to be replaced sooner than silicone breast implants.
How to Choose the Best Breast Implants
Breast Implant Shape vs Breast Implant Size
What matters the most, the shape or the size of your breasts following breast augmentation? Size and cc volumes of all styles of breast implants will be limited by the width of your chest wall. If you want a more natural breast shape, you may require anatomical ‘teardrop’ shaped breast implants. This will depend on how much breast tissue you have, the volume of the breast implant, and the breast implant placement you choose.
When breast size is more important than a natural result, high profile, non-anatomical breast implants are the most popular.
Large Breast Implants
Large breast implants tend to be considered anything over 500cc. The maximum silicone filled breast implants are 800cc. Breast implants over 800cc need to be custom made. The alternative is to have saline breast implants which can be overfilled to around 1000cc.
To avoid needing multiple breast augmentations if you want large breast implants and are small busted then you could consider tissue expanders otherwise referred to as expandable breast implants. They are filled with saline and have an external port which allows more saline to be added gradually. Depending on your plastic surgeon you may be able to have your tissue expanders overfilled to around 2000cc.
Find out more information about Extra Large Breast Implants and Extra Large Breast Augmentation
Incision options for Breast Implants
Selecting the incision option for breast augmentation is important not only because it is where the scar will be. The incision option will also affect the placement and can limit the size and shape of the breast implants that can be used.
Inframammary Incision
The inframammary incision is positioned in the natural crease under the breasts. This gives the surgeon the best access to the breast tissue and makes it easier to create a correctly sized pocket to accommodate, larger breast implants if desired. The inframammary incision is associated with more accurate placement of breast implants and lower infection rates and reduced hematoma and capsular contraction rates.
Transaxillary Incision
The transaxillary incision is made in the armpits. This limits access to breast tissue which makes it more challenging to create the pocket low and centrally enough. One significant advantage with the transaxillary incision for breast augmentation is the absence of any tension on the incision and scars that are well concealed away from the breasts. Infection rates, hematoma, and capsular contraction rates, are higher with the transaxillary incision.
Peri-areolar Incision
The peri-areolar incision is made around the outer edge of the bottom crescent of the areola. This allows the surgeon good access to breast tissue. The main disadvantage with the peri-areolar incision is visible scars if they don’t heal well. Like the transaxillary approach, placement may not be as accurate. Infection, hematoma, and capsular contraction rates are also higher.
Transumbilical Incision
Transumbilical Breast Augmentation (T.U.B.A) uses an incision made inside the belly button. This technique can only be performed with saline-filled, breast implants. Once healed there are no visible scars. T.U.B.A can make placement challenging and is not offered by all plastic surgeons.
Breast Implant Placement Options
Subglandular ‘Above The Muscle’
Subglandular breast augmentation is often referred to as ‘above the muscle’ breast augmentation. This means the breast implants sit where there would naturally be breast tissue. A tighter cleavage can normally be achieved and women report experiencing less pain than with submuscular ‘beneath the muscle’ breast augmentation.
The subglandular placement may be chosen when large breast implants are desired as skin will stretch more than muscle. However, thin patients, with little or no breast tissue to cover their breast implants, are not good candidates for the subgandular placement option.
Opinion is divided as to which placement option produces a better aesthetic result in women with enough breast tissue to provide adequate coverage. The main drawback with the subglandular placement for breast augmentation, is the slightly higher associated risks of capsular contraction.
Submuscular ‘Beneath The Muscle’
Submuscular breast augmentation is often referred to as ‘beneath the muscle’ breast augmentation. This means the breast implants sit partially or fully under the pectoral muscle. Submuscular placement can limit the size of breast implants as the muscle will stretch less easily than skin. Problems with breast implants under the muscle are rare, although it is more extensive surgery. When the pectoral muscles are flexed the breast implants will move slightly and the breast shape will be impacted, momentarily.
There is a slightly, lower associated risk of capsular contraction with the submuscular placement for breast augmentation. Another advantage with submuscular placement is that the muscle provides an extra layer, making rippling and implant edges, less easy to see. This is especially important for thin women with little breast tissue.
The terms dual-plane one and two, refer to the level at which the pectoral muscle is separated from the breast. All submuscular breast augmentations are at least a dual-plane one, meaning that the pectoralis major muscle has been released across the entire length of the inframammary fold. With dual-plane two the muscle is released up to around the lower border of the areola.
Mammograms With Breast Implants
According to the American Cancer Society, both saline and silicone-filled breast implants interfere with mammograms. The FDA reports in a mammogram with breast implants, breast tissue is obscured by between 22% and 83%.
Breast implants rupture has been reported due to mammograms with both saline and silicone-filled breast implants.
Breast Implants and Breast Augmentation Drains
Depending on how your body responds to surgery you may require drains after breast augmentation. This is to prevent any delay in healing which may occur if seromas (accumulation of fluid) or hematomas (accumulation of blood) occur.
General or Local Anesthetic
General Anesthetic (GA)
General anesthetic is still the preferred choice for many plastic surgeons performing breast augmentation or breast augmentation revision surgery. Plastic surgeons who opt to use general anesthetic believe it gives them more control. If a complication does arise they are also not limited by time as the general anaesthetic can be topped up to last longer.
Local Anesthetic (LA)
Local anesthetic is becoming a popular option for initial breast augmentation. Many plastic surgeons believe using a local anesthetic reduces associated risks and leads to a quicker recovery.
One advantage with a local anesthetic is that the patient can see how large their breasts are after the breast implants have been positioned. This means the breast implants can be changed for a different size or shape of breast implants if the patient is not happy. A local anesthetic also gives patients complete control if breast implants are being filled with saline and means that the patient can ask for more saline if they are not satisfied with the breast shape and, or size.
A sedative can also be administered with a local anesthetic if the patient does not want to be conscious but still wants to benefit from the lower risks and quicker recovery time associated with a local anesthetic.
Breast Augmentation Risks and Complications
All surgery carries risks of:
- Bleeding
- Infection
- An allergic reaction to the anaesthetic
- A blood clot forming in the veins
Bruising and Swelling
A minor complication of breast augmentation is bruising and swelling. This can cause discomfort for a couple of weeks. The majority of bruising should have gone within a month and almost of swelling within three months.
Infection
Infection can be a result of contaminated breast implants, poor hygiene and unhygienic facilities. The risk of infection is also increased when tissue expanders are filled with saline following placement. Infection after breast augmentation is usually treated with oral antibiotics, when it is severe then intravenous (IV) antibiotics may be required. Occasionally breast implants will need to be removed to allow an infection to clear up. Usually they can be replaced with new breast implants within a few months, after the infection has gone.
Necrosis
Necrosis is the formation of dying skin cells or tissue around the breast. The risk of necrosis increases with infection, use of steroids in the surgical breast pocket, large breast implants and smoking.
Necrosis can normally be treated with intravenous (IV) antibiotics, however, sometimes it will be necessary to remove the breast implants. A secondary breast augmentation procedure can usually be performed after a few months, as long as there is sufficient skin to cover the new breast implants.
Seromas and Hematomas
Both consist of a collection of fluid (seromas) or blood (hematomas) around the breast implant. They can cause swelling, pain and bruising. Either or both can occur soon after surgery, but hematomas may also be due to an injury, usually involving impact to the breast. The body may absorb small seromas and hematomas, however, larger ones may require a surgical drain.
Capsular Contraction
Once breast implants are in place, fibrous scar tissue forms around them, creating a tissue capsule. In some women, a tissue capsule forms that is unusually hard and dense. The capsule can also tighten and squeeze the implant. This condition is called capsular contracture, it may cause chronic pain and distort the shape of the breasts.
Symptoms of capsular contracture can start to appear as early as a few months after breast augmentation or breast reconstruction surgery or it can occur years later. Causes are unknown but the risk of capsular contracture increases with larger breast implants, subglandular placement, and if the pocket is not correctly sized.
Breast Tissue Atrophy
Breast tissue atrophy can occur with breast implants or even following breast implant removal. Causes include breast implants that are too large and, or heavy which causes the skin to become thinner and shrink over time.
Nerve Damage
Nerve damage caused during the procedure or over time can result in the nipples and, or areas of the breast becoming, less sensitive, or completely numb; this can be temporary or permanent. Causes include poor surgical techniques and, or breast implants that are too large.
Keloid Scarring
A keloid is a type of bulky scar that develops in the skin. Make sure you tell your surgeon that you have a tendency for keloid scars. This will allow for certain steps to be taken to minimise the chances of getting a keloid postoperatively. Keloid scars can develop at anytime (sometimes years) after surgery and may start or stop growing at any time.
Causes of keloid scars include:
- Tension across the scar, which explains the increased chance for keloid formation with the inframmary incision
- Family history/genetics
- Young age
- Darker skin type
- Hormonal upsurges and systemic diseases including thyroid problems, hypertension
Breast Implant Wrinkling and Folding
Breast implant types vary, they can wrinkle and, or fold under the skin. Typically this is associated more with saline breast implants that have a lower viscosity than silicone This may allow lower-pole expansion and settling and hence, wrinkling. Insufficient filling in saline implants may also contribute to the problem, in addition to shell folds and movement of filler material.
Other causes of visible ripples and breast implant edges include:
- Thin skin and lack of breast tissue, especially in the lower outer pole
- Subglandular placement
- Saline-filled breast implants
Breast Implant Extrusion
Breast implant extrusion normally occurs within around a month after breast augmentation.
Causes of breast implant extrusion include:
- Breast implants that wrinkle beneath thin skin
- The skin has stretched too much and become too thin
- The breast implant used is too large, putting too much pressure on the skin.
- A severe infection
If your breast implants have already extruded or are about to extrude, they will need to be removed.
After breast implant extrusion, surgery to resolve the issue will depend on your individual situation. For instance, you may choose to have new breast implants, if you have enough healthy skin and tissue to support and cover the breast implants.
Your plastic surgeon might suggest that you have a tissue expander (which stretches the skin to make room for the final implant) inserted for a few months, or you may choose to keep a tissue expander in permanently. If you don’t have enough skin or the skin is very thin, the best option may be to reconstruct the breast with a flap of tissue from another place on your body; in some cases, your plastic surgeon may recommend a combination of breast implants with a flap procedure.
Breast Implant Rupture
Breast implant rupture can happen with saline and silicone breast implants. Saline breast implant rupture will result in immediate deflation and the saline is safely absorbed and expelled in urine. Silicone breast implant rupture may not be detectable and can cause small, tender lumps (siliconomas).
Common breast implant rupture causes include:
- External injury to the breast
- Capsular Contraction
- Creasing/folding of the breast implant shell
- An inferior quality breast implant or when breast implants are damaged during breast surgery
Breast Implant Malposition
Breast implants will not always ‘settle’ as intended in the breast pocket created. This can result in a number of different complications. The most common breast implant misplacement issues are commonly referred to as double bubble and bottoming out. However breast implants can become displaced in any direction (laterally, medially, and less often superiorly) and often do so in an asymmetrical fashion, resulting in abnormal looking breasts.
Double Bubble
A double bubble is the term used to describe the unwanted appearance of a double curve in the lower half of the breast, following breast augmentation. This occurs when the lower edge of the breast implant sits below the pre-existing natural breast crease. In some women with small breasts the lower crease is very poorly defined or cannot be defined at all. If the upper breast tissue and skin stretches more easily over the breast implants, it may create a visible double curve in the lower half of the breast; hence the term ‘double bubble’.
Bottoming Out
This occurs when the breast implants move downwards outside of the pocket and can also result in displacement of the nipples, causing them to rise on the chest and, or point upwards. Although this can create a very ‘fake’ look, not all women feel unhappy with the appearance of their breasts when this occurs symmetrically.
Medial Displacement
Symmastia appears when breast implants displace medially giving the appearance of breasts that connect in the middle of the chest. This can be just the skin tenting anteriorly away from the breast plate (sternum), or it can be an actual connection between the breast implant pockets. Symmastia often does not become obvious until post-surgical swelling goes down.
Lateral Displacement
This occurs when breast implants slide too far to the side when standing or lying down. This may cause an unusual and unnatural appearance of the breasts or nipple/areola complex and, or leave a large gap between the breasts.
Superior Displacement
This occurs when breast implants sit too high on the chest wall. This can happen when they don’t settle enough or fail to stretch out the lower breast as much as expected.
Causes for breast Implant malposition include:
- Over dissection of breast tissue creating an incorrectly sized pocket for the implant
- Over dissection of the pectoral muscle
- Breast implants that are too heavy or too wide
- Breast implants positioned incorrectly
- Incorrect sizing of pockets and poor surgical technique
- When a breast lift is required
- Capsular contracture
Additional Complications and Risks of Extra Large Breast Implants
Associated risks and complications with extra large breast implants are an important issue around the ethics of providing breast augmentation with larger breast implants, typically over 800cc. When extra large silicone breast implants are used the size of the implants mean a bigger implant pocket needs to be created which can result in overdissection and a pocket that is actually too large for the breast implant cc volume.
Increased complications and risks associated with extra large breast implants include:
- Breast implant malplacement, in particular bottoming out and symmastia, also called uniboob (when breast implants meet in the middle of the chest).
- Slower wound healing which increases the risk of infection, necrosis and breast implant extrusion.
- Nerve damage which can cause nipple numbness and numbness in other areas of the augmented breasts.
- Breast tissue atrophy when skin becomes thinner, which can cause breast implant extrusion with extra large breast implants. This is because they are heavy which makes it more likely skin will become thinner and shrink over time.
- Excess sagging which may need to be corrected at a later date with mastopexy (breast lift) surgery, to improve the overall shape and look of breasts after extra large breast augmentation.
Breast Implants and Breast Feeding
Many women are able to breastfeed after breast augmentation, however, you should be willing to accept this may not be possible, before going ahead with breast augmentation.
Causes of not being able to breast feed with breast implants include:
- Dissection of milk ducts during the procedure, this can only happen with the peri-areolar (nipple) incision.
- Breast implants that are too heavy and put excess pressure on the milk ducts, making it difficult for milk to pass through easily (in the subglandular position).
Drains After Breast Augmentation
The drain is a narrow silicone or rubber tube, placed in the breast implant pocket. The drain allows fluid and, or blood that could build up in the pocket to drain away. Drains may be required regardless of the size of the breast implant or if it is filled with saline or silicone. Due to the creation of a larger raw surface of tissue, it is more likely they will be required with larger breast implants.
Drains can increase post-surgery discomfort and pain, this normally subsides when the drain is removed. Drains are also more likely to be required for breast augmentation revision procedures.
Drains may be used to treat infections. The drain helps to eliminate any significant accumulation of fluid around the breast implant which may also reduce the occurrence of a second infection.
Drain Bulb
The drain is accessible externally through a very small incision, and the end of the drain is connected to a small collection bulb. The bulb can be emptied and the contents measured at any given time. When the fluid coming out has decreased to a minimum, the drain tube will be removed.
Emptying Drains
Before you go home you will be shown how to periodically drain your bulbs. You will need to keep a record of the amount of fluid each time you empty them. This is important as it will guide your surgeon as to when it is safe to remove the drains.
Always wash your hands before and after each measurement. To start with drainage liquid should be bright red. This should change to a straw color after a few days and the amount of fluid should steadily decrease. You may need to empty your drains two to four times daily, or whenever they become approximately half full. After emptying your bulb, rinse it with water and gently compress it to make sure a vacuum is created when you close the system.
If you notice a slight increase in the amount of fluid, consider your activities during the day, it may be a sign that you need to take it easy for a few more days. A significant increase of fluid may be a sign that something is wrong and you should contact your surgeon immediately if this occurs.
If you need to keep in your drains when you go home is it worth wearing an appropriate drain management garment, with pockets or pouches where you can insert the bulbs to keep them secure. This helps to reduce the risk of the drains pulling on your wound site or possibly getting tangled up with clothes and, or long hair.
Risk of Infection
Drains provide bacteria with an access route out of your body. The risk of infection begins to increase rapidly after the drains have been in place for 21 days.
Signs of a drain-related infection include:
- A fever with a temperature of 101 degrees F (38.3 C) or higher
- Redness of your skin surrounding the drain
- Hardness or firmness where the drain exits your body
- Thickening rather than thinning of the drained liquid
- Foul smelling drainage or pus at the entry site
- Pain or discomfort at your drain sites
- A sudden change in the smell or colour of the drainage
Common drain problems include:
- Clots in the tubing, if this occurs, try gently kneading the area.
- Loss of vacuum pressure, if a proper vacuum isn’t created after emptying your bulb, your drain may fail to remove the fluid. This will cause a build-up up of fluid always seek advice if you are experiencing a higher level of discomfort than previously.
- Drain site infections which are more likely, the longer your drains are in place.
When to Call Your Consultant
You should call your surgeon if you have any concerns or questions at all, or if you develop any of the following problems:
- If your drainage is bright red for more than two or three days
- If you develop any signs or symptoms of an infection as noted above
- If a large amount of fluid is leaking from where the drain tubing is inserted into the surgical site
- If your drainage output suddenly decreases or stops abruptly
- If your drainage becomes thicker rather than thinner as time goes on
- If your bulb loses suction
- If your drain falls out
Removal of Drains Following Breast Surgery
Normally drains will be removed the day after breast augmentation. If you stay overnight in a hospital the drains will normally be removed before you leave. If you have had your procedure as an outpatient you may need to go back to the hospital or consultant’s office to have the drains removed. On occasion, it may be necessary for the drains to stay in, although for a straightforward breast augmentation it is unlikely they will remain in for longer than 48 hours.
Your consultant will remove your drains by cutting the suture holding them in place and gently pull out the tubing. This may cause some discomfort, however, this will normally only last a few minutes. Most people do not need any pain medications for this procedure. You will have small scars where the tubing exited your skin, but these usually fade and become almost invisible.
Recovery After Breast Augmentation
The day of surgery you will feel very sore and some discomfort, this is likely to be worse if you have submuscular breast augmentation or extra large breast implants. When you have a general anesthetic you may be kept in hospital overnight, especially if your surgery is planned for later in the day. Breast augmentation performed under local anesthetic, you will usually go home within a few hours of your procedure.
You may wake up with a sports bra on, if you are asked to bring one for the plastic surgeon to put on following the procedure. Some plastic surgeons recommend wearing a sports bra for a minimum of two weeks after a breast augmentation. You should move around as soon as possible to help prevent blood clots.
You may need between three and seven days off work and if you are in pain will be advised by your plastic surgeon about the painkillers, you should take. Normally after seven days the discomfort will have significantly reduced. Stitches that are not dissolvable will usually be removed around 10 to 14 days after a breast augmentation. Almost all plastic surgeons now use dissolvable stiches and they usually take around 10 to 14 days to dissolve. The first follow up consultation will usually be done to check your stitches have dissolved and ensure that everything is healing properly.
Breast Augmentation Recovery Timescale
The amount of swelling, bruising and pain you have after a breast augmentation will vary. It is important to rest for at least three days after to give your body a chance to recover from surgery. Most women find they can begin to start most of their usual daily activities within four to seven days.
- You should wait a minimum of one week before driving a car.
- Swimming should be avoided until your incisions have completely healed.
- Strenuous exercise and heavy lifting should be avoided for at least six weeks.
- Scars should begin to fade after around 12 weeks.
- At around 12 weeks the majority of swelling should have gone and your breasts should start to feel softer and may have dropped slightly.
- Around six months after almost all of the swelling will have gone and you will be able to get a good idea of how your breasts will look.
- After one year skin, tissue and muscles will have stretched and your breast implants should have settled into a nice position.
Breast Augmentation Cost
The cost of breast augmentation will typically depend on five key factors:
- Manufacturer and style of breast implants – breast implants cost on average between £700 and £1300 or $800 and $1400. Custom made silicone breast implants cost on average between £1000 and £1500 or $1100 and $1600.
- Type of procedure – T.U.B.A is typically more expensive than other breast augmentation procedures. Extra large breast implants over 800cc will usually cost more as the procedure will normally take longer and may require extra surgery such as an internal bra or additional permanent internal sutures. Tissue expanders, also referred to as expandable breast implants are usually more expensive and each additional “topping up” of tissue expanders will also have a charge.
- Facility – breast augmentation surgery performed in a hospital will cost more than when it is performed at the plastic surgeons facility.
- Anesthesia – general anesthetic will cost more as it requires an anesthetist who will also have an additional charge.
- Plastic surgeon – the experience and if a plastic surgeon is well known will usually be the main difference in the price of a breast augmentation. The more experienced or renowned a plastic surgeon is, typically the more they will charge.
Breast Augmentation and Cancer
Breast Implants and Cancer
The data indicates that breast implants do not cause breast cancer and there is no increased risk of breast cancer with breast implants.
Breast Implant Associated Large Cell Lymphoma – BIA-ALCL
Allergan has withdrawn certain styles of breast implants with textured shells due to a link with breast implant associated large cell lymphoma, BIA-ALCL. To date, the highest estimated risk is found with Allergan BIOCELL textured breast implants. The FDA and the MHRA do not recommend patients with Allergan BIOCELL textured breast implants have their breast implants removed, unless they show symptoms of BIA-ALCL.
Cosmetic Surgery Advancements with Breast Augmentation
Biplane Placement
The concept of the biplane muscle splitting technique was only introduced by Umar D. Khan in 2007. The breast implants are positioned both in front of and behind pectoralis major simultaneously without the need of muscle release. As the muscle-splitting technique only divides the medial two-thirds of the pectoralis major, this maintains the lateral portion of pectoralis major which can help prevent double bubble.
The biplane technique can also be used to correct cases of grade I and II ptosis with satisfactory lower pole fill and projection. In conclusion, this novel biplanar technique for breast augmentation optimizes the advantages of subglandular and submuscular breast augmentation, with simpler dissection and fewer complications than other submuscular techniques. It can be used for a wide variety of breast types with predictable results.
Botox (Neurotoxin) Assisted Breast Augmentation
This method is used for submuscular breast augmentation. After the muscle has been elevated, Neurotoxin is injected into the muscle before the breasts implants are positioned. This partially paralyzes the chest muscle, resulting in fewer muscle spasms that naturally occur during the healing process, and dramatically reduces discomfort following submuscular breast augmentation.
The other significant advantage is that by paralyzing the muscle, breast implants settle into position in about three to four weeks. This is much faster, compared to the usual three to four months it takes for breast implants in the submuscular placement, to settle into the desired position.
Trans Umbilical Breast Augmentation (T.U.B.A)
T.U.B.A was developed in 1991 by Dr Gerald Johnson and only requires a small incision in the belly button. Deflated breast implants are inserted and once they are in the correct location, they are filled to the required size with saline. To provide a view of the underlying tissues during this procedure, a tiny fiber-optic camera called an endoscope, is used to ensure that the breast implants are properly positioned.
T.U.B.A has the benefit of no visible scars as the only incision made is inside the belly button.
Because the pockets are formed by expansion as the breast implants are filled with saline, they conform to the shape of the breast implants. This eliminates any dead space that could harbour infection, hematomas or seromas.
Due to limited access and perspective, it is very difficult to control the position and shape of the pockets and to control any bleeding. This means a higher incidence of asymmetric breasts or a non-pleasing breast shape.
Internal Bra Technique
The utilisation of the internal bra technique for breast support with extra large breast implants, has been recognized as an effective method to reduce complications. As clinical experience has increased and new products are developed, the internal bra technique is offered by more plastic surgeons.
Dermal Fillers and Autologous Fat Transfer
Women that have rippling or breast implant edges may benefit from fat transfer as described in the information below. Newer generations of dermal fillers are also used by some surgeons to cover ripples and breast implant edges.
Breast Augmentation With Autologous Fat Transfer
Breast augmentation can be done without breast implants. This involves the transfer of fat and procedures are minimally invasive, using needles and require no incisions or stitches.
When the fat is not absorbed, the breasts can look and feel normal. Breast enlargement with autologous fat transfer is usually limited to one cup size. If more fat is injected than can be supported, the fat will be reabsorbed and possibly become harder. Additionally, fat resorption can cause misshapen breasts.
Fat may interfere with breast screening examinations: the volume of fat required to enlarge the breast makes the technique prone to calcifications. These calcifications will be visible on a mammogram. These changes will be present over a woman’s lifetime. The pattern of those calcifications is different from calcifications associated with breast cancer. However, they may result in the need for more frequent breast biopsies, especially if there is a strong history of breast cancer in the family. A lifetime of close monitoring and follow-up mammograms may be necessary.
Six Important Questions to Ask About Breast Augmentation
1. The Incision Option:
- Inframammary (in crease under breast)
- Transaxillary (armpit)
- Peri-areolar (nipple)
- Trans-umbilical (belly button)
2. Placement Option
- Subglandular (above the muscle)
- Submuscular (Dual Plane 1 or 2)
3. Breast Implant Shape
- Non-anatomical (round)
- Anatomical (tear drop)
4. Breast Implant Filling
- Saline
- Silicone
- Hydrogel
5. Breast Implant Shell
- Textured surface
- Smooth surface
6. Breast Implant Manufacturer
- Style
- CC Volume
Five Important Questions to Ask Your Plastic Surgeon Before Breast Augmentation
1. If they have any complaints registered against them with the GMC.
2. How many times they’ve performed this operation in the last year.
3. How many times they’ve had to do revision surgery following an initial breast augmentation (additional surgery to repair or change something they’ve already done).
4. Why they are recommending an incision and placement option.
5. Ensure you know the manufacturer and style and size of the implant being used.
My Breast Augmentation Journey
First Breast Augmentation
When I had my first consultation I explained my priority was shape over size and I wanted my breasts to look as natural as possible with implants. My consultant, Mr Mc George, recommended McGhan low profile, non-anatomical, 280cc silicone-filled breast implants. Three months later most of my swelling had gone and I had increased from a 32A to a 32C cup size. During my follow up appointment after six month later, my consultant advised I might have stage 1 capsular contraction and asked me to come back to see him in another three months.
Second Breast Augmentation
When I went back, around nine months after my initial breast augmentation, my consultant confirmed I had stage 1 capsular contraction. He could either remove the capsules and reinsert the same sized breast implants or I could have for larger breast implants. After hours of telephone conversations to discuss what type of breast implants would give me the natural looking results I was seeking, we agreed that I would have McGhan moderate profile, 395cc anatomical breast implants.
Three months after my second breast augmentation most of my swelling had gone and I had increased from a 32C to approximately a 32D cup size. Six months after my second breast augmentation I still knew I wanted larger breasts. Mr Mc George advised the only way he give me larger breast implants, would be if he used high profile, non-anatomical breast implants. The issue is they would look very round and fake. He mentioned that there were current development plans for the production of high profile, anatomical breast implants and they would give me a more natural shape. He did not know when they would be available and agreed to call me as soon as they were. Approximately nine months later I got his call.
Third Breast Augmentation
Mr Mc George offered to replace my current breast implants with McGhan high profile 535cc anatomical implants. Three months later, after many more telephone conversations, I decided to go ahead. The McGhan high profile 535cc anatomical breast implants finally gave me the size and natural shape I had been aiming for. As before after around three months most of my swelling had gone and I had increased from a 32D to a 32E cup size. (McGhan were taken over by Allergan.)
I am forever grateful, that I had a consultant that cared enough to spend hours talking to me and helped me to make the right decisions. My breast implants are almost 20 years old and my breasts still look great.
My Opinion
As breast implants constantly evolve new problems are always possible. Always be prepared to have more surgery and that at some point you may need revision breast augmentation. This is more likely with large breast implants as they will stretch the skin faster.
Breast implant illness (BII) refers to a range of symptoms reported by women with breast implants. The research shows that although BII is not recognized, it is possible that some people will have autoimmune conditions triggered or aggravated by breast implants. The most common symptoms of breast implant illness are joint pain, headaches, chronic fatigue and “brain fog”.
Although there is no evidence that silicone or oils improve scars, I highly recommend using silicone strips. I used them after my second and third breast augmentations and my scars are flatter and finer, than they were after my first breast augmentation.
Annabelle Baugh | Founder